Guide to Ulcerative Colitis


What Is Ulcerative Colitis?
Ulcerative Colitis is a type of bowel disease that causes long-term inflammation of the cells that line your rectum and colon (also called the large intestine). This may lead to sores called ulcers that can bleed and keep your body from digesting food like it should. You can take medicine to calm the inflammation and learn ways to ease its effects on your daily life.

Warning Sign: Abdominal Pain
A belly ache and diarrhea with blood or pus in it could be warning signs of ulcerative colitis. Some people have mild symptoms every once in a while, but others have worse symptoms more often.

Warning Sign: Weight Loss
The long-term inflammation that comes with UC can cause digestive problems. These could lead to:
- Weight loss
- Poor appetite
- Nausea
- Lack of growth in children

Other Warning Signs
Some people with ulcerative colitis have symptoms outside the digestive system. These may include:
- Joint pain
- Skin sores
- Fatigue
- Anemia (low red blood cell count)
- Frequent fevers

Ulcerative Colitis or Crohn's?
Ulcerative colitis symptoms are similar to those of another inflammatory bowel condition called Crohn's disease. UC only affects your large intestine. But Crohn's can happen anywhere in your digestive tract. It can cause symptoms from your mouth to your anus. Another disease called irritable bowel syndrome can cause long-term belly pain and diarrhea, but it doesn't lead to inflammation or sores in your intestines.
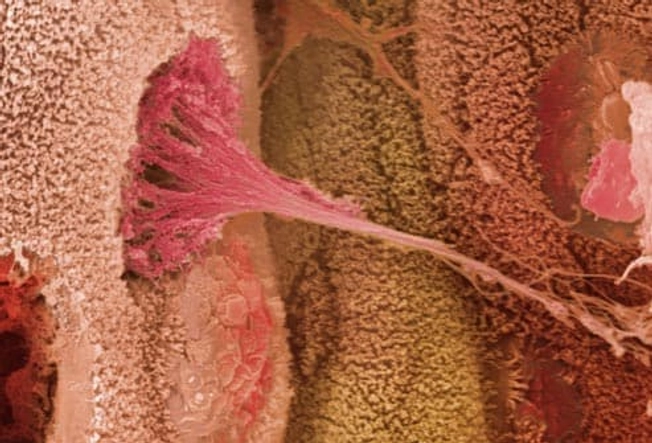
What Causes Ulcerative Colitis?
The exact cause isn't clear. But researchers think your immune system -- which defends you from germs -- is involved. When you have UC, your immune system may not react like it should to bacteria in your digestive tract. Doctors aren't sure whether this triggers the condition or results from it. Stress and your diet can make your symptoms worse, but they don't cause ulcerative colitis.

Diagnosing Ulcerative Colitis
To diagnose ulcerative colitis, your doctor will do a colonoscopy. They’ll insert a tiny camera into your rectum to get an up-close look at the inside of your colon. This helps them spot inflammation or ulcers in the area. A colonoscopy can also help your doctor rule out other conditions like Crohn's disease and cancer.

Do UC Symptoms Go Away?
Your UC symptoms will come and go. The disease can go into remission, which means you may have no symptoms for long periods of time. Remission can last for months or years, but the symptoms will return.

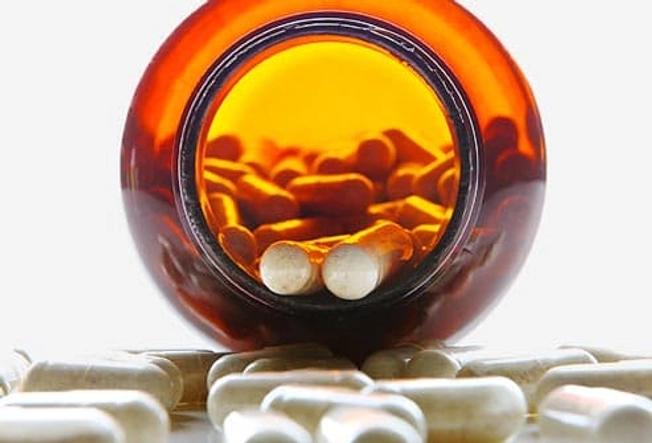
Medications for Ulcerative Colitis
Medications can calm the inflammation inside your colon. The first one you’ll usually try is from a group called aminosalicylates. If that doesn't help, your doctor might prescribe a steroid like prednisone. A third option is an immune modifier, which lowers inflammation by changing the activity of your immune system. It can take up to 3 months before you feel the benefits.

Biologic Therapies
If other medicines don’t help, your doctor may suggest one of a group of medications called biologics. They help your body destroy proteins linked to inflammation. You usually get them in an IV. Another type of treatment is JAK inhibitors, which travel quickly through your bloodstream to block inflammation. You’ll take these as a pill.

Surgery for Ulcerative Colitis
Up to 45% of people with ulcerative colitis will need surgery, either to repair a tear or remove a severely damaged colon. Your UC won't come back after the surgeon removes your colon. Newer surgical techniques mean you may not need a colostomy bag to get rid of waste.

Urgent Care for Ulcerative Colitis
The disease can sometimes cause problems that send you to the hospital. These may include a bleeding ulcer or severe diarrhea that causes dehydration. If this happens to you, doctors will stop the loss of blood and other fluids. If there’s a tear in your colon, you may need surgery to fix it.

Ulcerative Colitis and Colon Cancer
Your risk for colon cancer goes up if you have UC. It depends on how much of your colon is involved and how serious it is. The odds also rise after you've had UC for 8-10 years -- and they go up over time. Treatment that puts your UC in remission may also make cancer less likely. Colonoscopy screening helps doctors find colon cancer early, when it's easier to treat.
- Use websites and cellphone apps to find restrooms in airports, train stations, or other large venues ahead of time.
- Carry extra underwear and wet wipes.
- Bring enough medication to last the entire trip, along with copies of your prescriptions.
- Tell your doctor about your plans to see if you need to take other precautions.

Other Health Problems
Some people with ulcerative colitis get conditions like osteoporosis, arthritis, kidney stones, and eye problems such as uveitis. It’s rare, but UC can also lead to liver disease. Researchers think these problems result from the widespread inflammation. They may improve when you treat your UC.

Living With UC: Reducing Flares
Triggers like stress, smoking, missing doses of medication, and eating certain foods can make your symptoms worse. Once you know your triggers, you can avoid them. If flares continue, talk to your doctor about a change in your treatment plan.

Living With UC: Diet Changes
Diet doesn't cause ulcerative colitis, but some foods may make your symptoms worse. Common ones include dairy, fatty foods, and foods with too much fiber, which can trigger diarrhea. It can help to keep a journal of what you eat and any symptoms you have. Look for links and avoid triggers. If you lose a lot of weight, you may need to work with a dietitian to come up with a healthy diet.
Living With UC: Supplements
Ulcerative colitis often causes bleeding in your colon, which can lead to a shortage of iron in your body. Some medications you take to treat UC can affect the way your body absorbs nutrients like folic acid and calcium. Ask your doctor if you need to take supplements.

Living With UC: Probiotics
These "friendly" bacteria are similar to those that live in your intestine and prevent the growth of too many harmful bacteria. We need more research to know if probiotics can help with ulcerative colitis. You can find probiotics in some yogurts, milk, tempeh, and soy beverages. Or you can buy them as supplements.

Living With UC: Staying Hydrated
Long-term diarrhea puts you at risk of dehydration, which can lead to weakness and kidney problems. To stay hydrated, drink plenty of water. Check with your doctor to see how much fluid you need.

Living With UC: Relationships
You don't have to let ulcerative colitis get in the way of intimacy. Talk to your partner about how your symptoms affect you and any concerns you have. You might want to see a therapist who specializes in long-term illness. Talk to your doctor if sexual problems become an issue.

Living With UC: Travel
With a little extra planning, most people with ulcerative colitis can travel comfortably. Follow these steps:
- Use websites and cellphone apps to find restrooms in airports, train stations, or other large venues ahead of time.
- Carry extra underwear and wet wipes.
- Bring enough medication to last the entire trip, along with copies of your prescriptions.
- Tell your doctor about your plans to see if you need to take other precautions.
IMAGES PROVIDED BY:
1)VEM/Photo Researchers
2)ISM/Phototake
3)Peter Cade/Stone
4)Corbis/Photolibrary
5)David Musher/Photo Researchers
6)SPL/Photo Researchers
7)BSIP/Phototake
8)Comstock
9)Lauren Nicole/Digital Vision
10)Altrendo Images
11)Clerkenwell/Agency Collection
12)Xavier Bonghi/Stone
13)ISM/Phototake
14)MedicImage
15)Comstock
16)Mario Matassa/Fresh Food Images
17)Clerkenwell/Agency Collection
18)Shelia Paras/Flickr
19)Steve Pomberg/WebMD
20)Imagebroker/Photolibrary
21)Nick Koudis/Photodisc
22)Bernard van Berg/Iconica
23)Eddie Hironaka/Photographer’s Choice
SOURCES:
Crohn's & Colitis Foundation of America: "Complementary and Alternative Medicine," "Diet and Nutrition," "Living with UC," "Managing Flares and Other IBD Symptoms," "Surgery for Ulcerative Colitis," "The Intimate Relationship of Sex and IBD."
Medicine: "Trichuris suis ova therapy in inflammatory bowel disease."
National Digestive Diseases Information Clearinghouse: "How is Ulcerative Colitis Diagnosed?" "Irritable Bowel Syndrome," "Is Colon Cancer a Concern?" "Ulcerative Colitis," "What Are the Symptoms of Ulcerative Colitis?" "What Causes Ulcerative Colitis?" "What is the Treatment for Ulcerative Colitis?"
Scanning Microscopy: "Renal stone formation in patients with inflammatory bowel disease."
World Journal of Gastroenterology: "Remission induction and maintenance effect of probiotics on ulcerative colitis: a meta-analysis."