An early-stage HER2-positive (HER2+) breast cancer is always a shock, but today’s treatment options should give you hope. Over the past 2 decades, advances in medicine have brought us new, effective therapies.
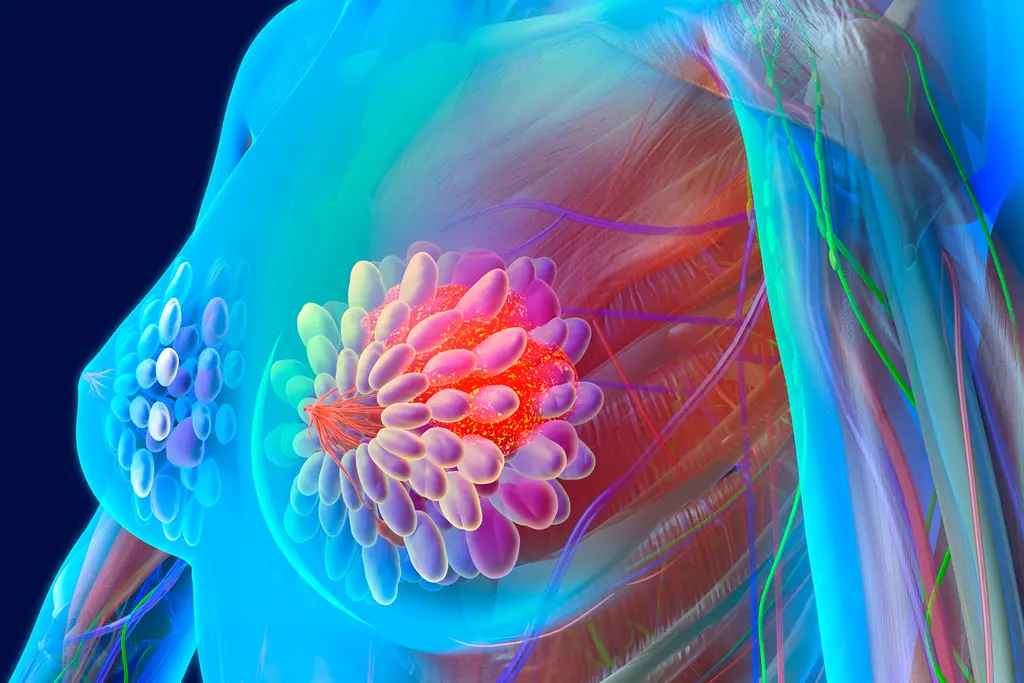
About one in five people with breast cancer have the HER2+ subtype. If your breast cancer is of the HER2+ subtype, your tumor has high levels of a protein called human epidermal growth factor receptor 2 (HER2). HER2 plays a role in the growth of cancer cells, which is why HER2+ breast cancer tends to be aggressive.
Treatment Terms
When your health care team talks about your HER2+ breast cancer treatment, they may use terms you don’t know. These are some common ones and what they mean.
- Neoadjuvant: Refers to treatment given before surgery. The goal is to shrink the tumor before removing it.
- Adjuvant: Refers to treatment given after surgery. The goal is to destroy cancer cells that might remain in the body.
- Targeted therapy: Medication that blocks the growth of specific cancer cells. It interferes with molecules that help them grow and survive.
- Chemotherapy: Drugs that destroy cancer cells.
- Endocrine therapy: Medications that lower estrogen levels or block the actions of estrogen.
- Biologic: A cancer medicine made from a living organism or the products of a living organism, such as proteins, sugars, or even cells and tissues.
HER2+ Treatment Strategies
Treatment for early-stage HER2-positive breast cancer will likely include some combination of surgery, targeted therapy, chemotherapy, and possibly other therapies. What’s right for you will depend on your wants and needs. There are three typical treatment strategies:
- Most common: neoadjuvant chemotherapy plus HER2-targeted therapy. Most people with HER2+ breast cancer, including those with very small tumors, use this plan. After surgery, they’ll get adjuvant therapy with HER2-targeted therapy.
- Less common: surgery, followed by adjuvant treatment with chemotherapy and HER2-directed therapy. Some people, especially those with small tumors, will take this strategy.
- Hormone-driven. If your cancer is hormone receptor-positive, your doctor may also offer you endocrine therapy. It’s a daily pill taken for at least 5 years after you finish chemo.
Targeted Therapy: Herceptin
Trastuzumab (Herceptin) was the first targeted therapy approved by the FDA for HER2+ breast cancer. It’s a type of biologic drug called a monoclonal antibody.
Trastuzumab is given intravenously (with an IV) weekly or every 3 weeks. As an adjuvant therapy, one year of treatment of treatment is typical.
Multiple studies show that trastuzumab can dramatically improve survival. In fact, trastuzumab-based treatments for HER2+ breast cancer are considered the gold standard. The main downside is cost. Without insurance, a year of trastuzumab could set you back at least $70,000.
Targeted Therapy: Herceptin Biosimilars
Generic drugs don’t exist for brand-name biologics. Biologics are made of large, complex molecules and produced -- thanks to the magic of biotechnology -- in a living system, such as an animal or plant cell. You can’t replicate that.
But you can create a similar version. These drugs are called biosimilars. They have “no clinically meaningful differences” in terms of safety, purity, or potency.
Trastuzumab and hyaluronidase (Herceptin Hylecta) is another type of trastuzumab treatment that is injected underneath the skin.
Targeted Therapy: Perjeta
Pertuzumab (Perjeta) treats HER2-positive early breast cancer, usually in combination with trastuzumab and chemotherapy. It’s FDA-approved for neoadjuvant and adjuvant treatment.
- Neoadjuvant use: For people with HER2+ breast cancer that is locally advanced, inflammatory, or early-stage.
- Adjuvant use: For people with HER2+ early breast cancer that’s highly likely to come back.
For people who are receiving a combination of targeted therapy, the drug trastuzumab, pertuzumab and hyaluronidase (Phesgo) may be given as a shot under the skin.
Targeted Therapy: Kinase Inhibitors
Kinase inhibitors block the action of HER2 and other kinase proteins that help cancer cells grow.
Neratinib (Nerlynx) is a kinase inhibitor used to treat HER2-positive early breast cancer after receiving a year of trastuzumab. It is a pill that is taken daily.
Other Treatments
Targeted therapy has helped people with HER2+ breast cancer live longer and have a better quality of life. But other therapies could also be part of your treatment:
- Chemotherapy. You’ll get chemo in cycles. One day you’ll get the treatment, and then you’ll wait 14 or 21 days for the next treatment. This gives your body a chance to recover from the side effects. As an adjuvant therapy, expect to start within 4 to 6 weeks of surgery.
- Endocrine therapy. More than half of breast cancers feed on estrogen to grow. (The other half can grow without it.) If your cancer is estrogen-dependent, endocrine therapy can cut off or limit the cancer cells’ estrogen “food supply.”
- Radiation therapy. A beam of high-energy X-rays can slow or stop cancer cell growth. You may get radiation therapy after surgery to lower the chances of a tumor coming back either in the breast or chest wall.
- T-DM1, or ado-trastuzumab emtansine (Kadcyla). This drug combines trastuzumab with an anticancer drug called DM1. For early breast cancer, your doctor may prescribe it as an adjuvant therapy if:
- You’ve already had neoadjuvant therapy with trastuzumab and a taxane (chemotherapy)
- You still show signs of remaining invasive cancer (residual cancer)
Show Sources
Photo Credit: FatCamera / Getty Images
SOURCES:
Signal Transduction and Targeted Therapy: “Targeted therapeutic options and future perspectives for HER2-positive breast cancer.”
UpToDate: “Patient education: Treatment of early HER2-positive breast cancer (Beyond the Basics).”
World Journal of Clinical Oncology: “Targeted therapies in breast cancer: New challenges to fight against resistance.”
American Journal of Managed Care: “Integrating Trastuzumab Biosimilars and HER2-Directed Therapies into HER2-Positive Breast Cancer Management.”
Medical Oncology: “Biosimilars for breast cancer: a review of HER2-targeted antibodies in the United States.”
FDA: “What Are ‘Biologics’: Questions and Answers,” “Biosimilar and Interchangeable Products.”
Perjeta: “Important Safety Information/Indications.”
National Cancer Institute: “Definition: Biologic.”
National Cancer Institute: “T-DM1 Approval Expanded to Include Some Women with Early-Stage HER2-Positive Breast Cancer.”
Global Journal of Health Science: “Cost-Effectiveness Analysis of Trastuzumab in the Adjuvant Treatment for Early Breast Cancer.”
American Cancer Society: “Targeted Drug Therapy for Breast Cancer.”