- Overview & Types
- Symptoms & Diagnosis
- Treatment
- Living With
- Related Conditions
- Type 2 Diabetes
- Type 1 Diabetes
- Gestational Diabetes
- Appointment Prep
- View Full Guide
What to Do About Diabetic Peripheral Neuropathy


What Is It?
Nerve damage, what doctors call neuropathy, is a common complication of both type 1 and type 2 diabetes. Peripheral means the nerves in your feet, hands, legs, or arms are affected. Diabetic peripheral neuropathy (DPN) can feel like tingling, burning, pins and needles, stabbing, or even numbness. If you're also overweight or have high blood pressure, high triglyceride levels, or plaque buildup in your heart's arteries, your odds of DPN go up.

Manage Your Numbers
High blood sugar over time damages nerves and the small blood vessels that support them. When your blood sugar level is consistently in the normal range, you lower the chance of complications like DPN and help stop it from getting worse. Follow your doctor's instructions about taking medicine or insulin as well as other steps to control your glucose.

Exercise
Moderate physical activity can delay problems and even reverse symptoms. Aside from that, it helps your balance and strength, so you're less likely to fall. Adults shouldn't skip exercise for more than 2 days in a row and get a total of at least 150 minutes a week. Brisk walks are a great way to start if you aren't working out regularly yet.

Stop Smoking
It's linked to low oxygen in your blood, which means tissues like your blood vessels and nerves may not get enough oxygen either. It also creates "free radicals" that can damage cells, harms the lining of blood vessels, makes it harder to control your blood sugar, and causes inflammation. All of this can lead to DPN or make it worse.

Eat Healthy
Fruits, vegetables, whole grains, low-fat dairy, lean proteins, fish, and high-fiber and low-salt foods are good for you whether you have diabetes or not. Good nutrition helps keep your body strong and working well. That includes your nerve endings and blood vessels. Eating well is also important to manage your weight and blood sugar.

Vitamins D and B12
People who don't get enough of these tend to develop DPN. Sunlight is a good source of vitamin D, as are cheese, egg yolks, mushrooms, and fatty fish like tuna, salmon, and mackerel. Fish and red meat have vitamin B12. Some foods have these vitamins added, too, like orange juice, soy milk, and cereals. Taking vitamin D supplements when you have DPN may ease symptoms, but it doesn't look like B12 supplements help.

Medication
Over-the-counter pain relievers like ibuprofen don't usually work for DPN. But some prescription medicines that treat depression and seizures -- including duloxetine, gabapentin, pregabalin, and tricyclic antidepressants -- might make it hurt less. You often take them at night so you sleep better. They can have unpleasant side effects though, so talk to your doctor about what the right choice is for you.

Capsaicin
Put it on your skin in a cream, ointment, or patch, and it breaks down substances in nerve endings around there so they can't send pain signals. One study found that people who used a capsaicin patch one time for 30 minutes had pain relief and slept better for up to 12 weeks. This is the chemical that makes peppers hot, and it can burn a little when you apply it.

Supplements
More research is needed, but early studies suggest that the antioxidants alpha-lipoic acid (ALA) and acetyl-L-carnitine may protect and repair nerves and lessen pain. Check with your doctor before you start taking these because they can cause problems for some people and with some medications.

Acupuncture
One study found it to be better than traditional medication for DPN symptoms, and typically with few side effects. It may work by triggering your body to use the energy and chemistry of your immune system to help heal and reduce pain. Look for a certified practitioner if you want to try it.

Relaxation and Meditation
Practices such as yoga, massage, guided imagery, deep breathing exercises, tai chi, even hypnosis can help lower your heart rate, blood pressure, and other signs of stress that make chronic pain and discomfort harder to manage. Scientific results are mixed, but many people find these types of complementary treatments effective.

Essential Oils
Extracts from plants including rosemary, lavender, eucalyptus, chamomile, and peppermint can be rubbed on your skin or used in aromatherapy to manage pain. They may also ease the stress that comes from dealing with a condition that can't be cured. A word of caution: When you put essential oils directly on your skin, they probably should be mixed with another oil to dilute them.

Treat Your Feet Gently
Because nerve damage can make it harder to tell when something's wrong, try to avoid injuring your feet. Don't walk around barefoot. Make sure your shoes fit properly, and break new ones in slowly. Wear a fresh pair of cotton socks each day. Be careful trimming toenails. Check your feet daily for cracks, blisters, and sores; get a full professional exam at least once a year.

Warm Bath With Epsom Salts?
Although it may be soothing, it's not recommended. Soaking can dry your skin, cause irritation, and open cracks that could become infected. You might also scald your skin in water that's too hot.
You should still wash your feet in lukewarm water every day.

Biofeedback
Chronic pain is one of several conditions this therapy is used for. While you learn relaxation techniques, your vital signs, like heart rate and blood pressure, are tracked with sensors. You see your results on a screen so you can tell how well you're doing. You work toward getting the same results without the monitoring equipment.
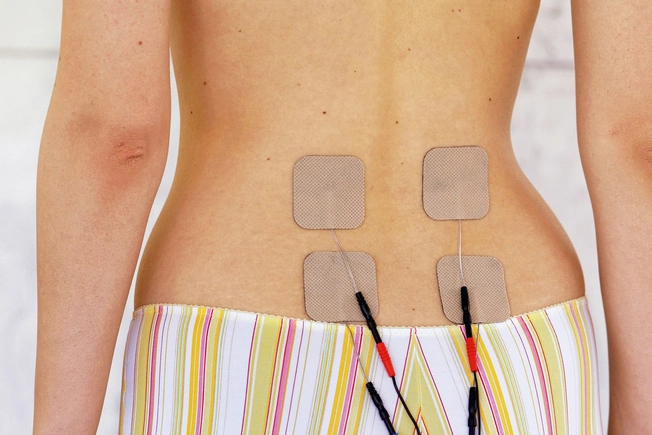
TENS
For severe pain, your doctor might suggest transcutaneous electrical nerve stimulation. You use a device that sends small electrical pulses through your skin either near where it hurts or at your spine. The idea is to block or confuse the pain-triggering messages your body is sending to your brain. It's generally safe, but there's little evidence this treatment is effective for DPN.
IMAGES PROVIDED BY:
1) spukkato / Thinkstock
2) AndreyPopov / Thinkstock
3) blyjak / Thinkstock
4) icefront / Thinkstock
5) Lisovskaya / Thinkstock
6) (Left to right) Janie Airey / Thinkstock, nehopelon / Thinkstock
7) smartstock / Thinkstock
8) danielle71 / Thinkstock
9) John Foxx / Thinkstock
10) Blend RF / Jon Feingersh
11) Ridofranz / Thinkstock
12) Amy_Lv / Thinkstock
13) nito100 / Thinkstock
14) Madiz / Thinkstock
15) Will & Deni McIntyre / Science Source
16) doc stock RM / Pro Health Media / Medical Images
SOURCES:
UpToDate: "Patient education: Diabetic neuropathy (Beyond the Basics)," "Patient education: Nerve damage caused by diabetes (The Basics)."
Cleveland Clinic: "High Blood Sugar Is Toxic to Your Nerves — Here's How to Avoid It."
BMC Neurology: "Potential risk factors for diabetic neuropathy: a case control study."
National Institute of Diabetes and Digestive and Kidney Diseases: "Peripheral Neuropathy," "Relaxation Techniques."
Journal of Diabetes and Its Complications: "Exercise training can modify the natural history of diabetic peripheral neuropathy."
Clinical Therapeutics: "Declining Skeletal Muscle Function in Diabetic Peripheral Neuropathy."
Clinical Diabetes: "Standards of Medical Care in Diabetes—2015 Abridged for Primary Care Providers."
Journal of General Internal Medicine: "The Effect of Cigarette Smoking on Diabetic Peripheral Neuropathy: A Systematic Review and Meta-Analysis."
Journal of Clinical and Translational Endocrinology: "The association between vitamin D level and diabetic peripheral neuropathy in patients with type 2 diabetes mellitus: An update systematic review and meta-analysis."
Singapore Medical Journal: "Vitamin B supplementation for diabetic peripheral neuropathy."
Mayo Clinic: "Diabetic neuropathy: Can dietary supplements help?" "Diabetes care: 10 ways to avoid complications."
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy: "Guidelines in the management of diabetic nerve pain: clinical utility of pregabalin."
British Journal of Anaesthesia: "Topical capsaicin for pain management: therapeutic potential and mechanisms of action of the new high-concentration capsaicin 8% patch."
Chinese Acupuncture & Moxibustion: "Acupuncture for distal symmetric multiple peripheral neuropathy of diabetes mellitus: a randomized controlled trial."
Journal of Alternative and Complementary Medicine: "Acupuncture for the Treatment of Peripheral Neuropathy: A Systematic Review and Meta-Analysis."
National Center for Complementary and Integrative Health: "Chronic Pain: In Depth."
Journal of Pharmacy & BioAllied Sciences: "Alternative therapies useful in the management of diabetes: A systematic review."
American Journal of Clinical Dermatology: "Dermatological care of the diabetic foot."
American Diabetes Association: "Foot Complications."
Foundation for Peripheral Neuropathy: "Biofeedback Therapy."
Diabetes Research and Clinical Practice: "Effect of transcutaneous electrical nerve stimulation on symptomatic diabetic peripheral neuropathy: a meta-analysis of randomized controlled trials."
Cochrane: "Transcutaneous electrical nerve stimulation (TENS) for neuropathic pain."
Drugs: "Capsaicin 8% Dermal Patch: A Review in Peripheral Neuropathic Pain."